Abstract
Introduction Fms-like tyrosine kinase 3 internal tandem duplication (FLT3-ITD) mutations are observed in about 30 % of patients with newly diagnosed cytogenetically normal acute myeloid leukemia (CN-AML) and has now been acknowledged to be associated with a poor survival. However, long-term follow-up revealed a high degree of heterogeneity in the clinical prognosis of these patients. Further risk stratification to identify high-risk patients is urgently needed.
Methods A total of 106 patients with CN-AML and FLT3-ITD mutations who visited the People's Hospital of Peking University from 2007-2019 were included, and target region sequencing was performed by 266 gene panel. Patients were randomly divided into training and validation cohort according to the ratio of 7:3. Molecular and clinical data in training cohort were incorporated to construct a nomogram model. Cumulative incidence of relapse (CIR), Relapse-free survival (RFS) and survival by allogenic hematopoietic stem cell transplantation (allo-HSCT) and consolidation chemotherapy were compared.
Results Clinical variables, genes, and genetic groups with mutations occurring in more than 10 patients were enrolled for univariate analysis of RFS (allo-HSCT was recorded as a censored event). And to avoid bias patients with RFS ≤ 4.57 months (median interval from complete remission to allo-HSCT) would be excluded from the subsequent analyses unless receiving an allo-HSCT was treated as a censored event. Three variables were eventually entered into the nomogram analysis: DNMT3A mutation (+ vs. -), minimal residual disease detected by multiparameter flow cytometry (MPFC-MRD) at the end of the 2nd course of consolidation chemotherapy (CON2) (+ vs. -, represents ≥ vs. <0.01%), typical ITDs (+ vs. -, represents ITDs have insertion sequences that exactly match wild-type FLT3 gene vs. ITDs have insertion sequences containing other exogenous nucleotides). And the model demonstrated good discrimination in both the training and validation cohort with C-index value of 0.82 (95% confidence interval, 0.7-0.86), 0.86 (95% confidence interval, 0.76-0.95), respectively.
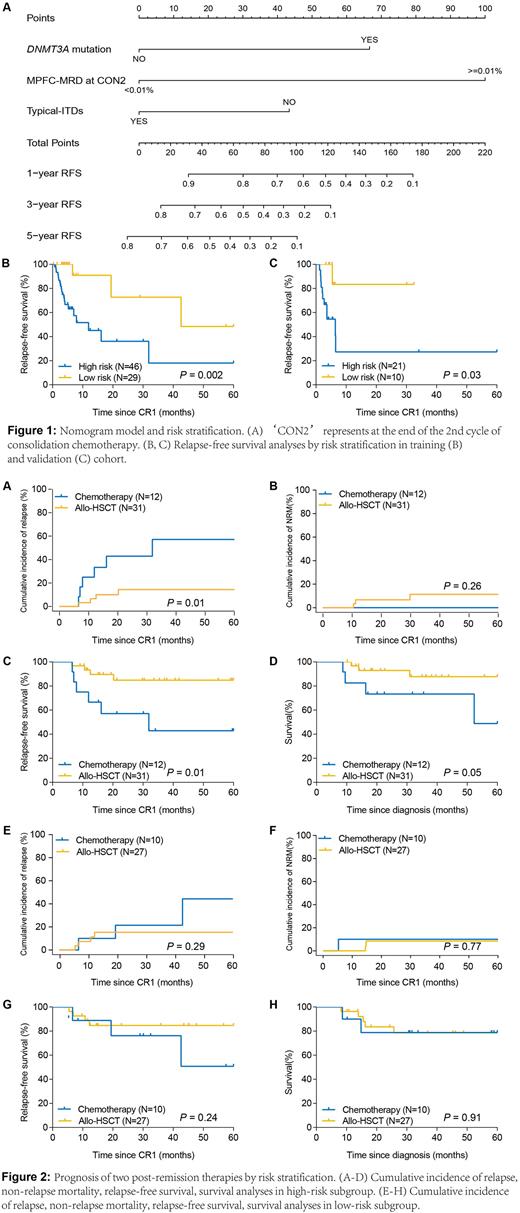
The Nomogram model was constructed as: Score = 1.44×DNMT3A mutation+2.16×MFPC-MRD-0.94×typical ITDs (Figure 1, A). According to the variables in nomogram model, patients with risk scores ≤ 0 were assigned to the low-risk subgroup (N = 39) and the rest were assigned to the high-risk subgroup (N = 67). The 5-year RFS was significantly higher in the low-risk group than in the high-risk group (training cohort, HR 3.68 [1.16-11.66], P = 0.002; validation group, HR 4.45 [1.52-13.00], P = 0.03) (Figure 1, B-C).
We then interrogated the effect of consolidation chemotherapy and allo-HSCT as post-remission therapies in the two risk subgroups. Allo-HSCT did not further improve the prognosis of patients in the low-risk group (allo-HSCT vs. chemotherapy, 5-year CIR, HR 0.46 [0.11-1.93], P = 0.29; 5-year RFS, HR 0.41 [0.09-1.86], P = 0.24; 5-year survival, HR 0.91 [0.18-4.68], P = 0.91) (Figure 2, A-D). In contrast, in the high-risk group of patients, transplantation showed a significant survival benefit (5-year CIR, HR 0.21 [0.06-0.74], P = 0.01; 5-year RFS, HR 0.23 [0.06-0.80], P = 0.01; 5-year survival, HR 0.25 [0.06-1.11], P = 0.05) (Figure 2, E-H).
Conclusion Our study suggests that risk stratification by our novel nomogram scoring system can identify patients at high risk of relapse in CN-AML with FLT3-ITD mutations and allo-HSCT further benefits their prognosis.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.